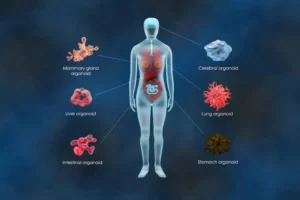
Xenograft models are used extensively in cancer research to simulate the disease’s progression, behavior, and response to treatment. They involve transplanting human cancer cells into immunocompromised mice, providing a controlled environment to study human cancer1. Depending on the research objectives and model type, the transplanted cells may be primary patient-derived tumor or leukemia cells or established cell lines derived from these samples.
Patient-derived xenografts (PDX) involve transferring tumor or leukemia cells directly from a patient into an immunodeficient mouse. PDX models retain the original tumor’s histological and genetic features, making them ideal for studying tumor progression2.
Cell line-derived xenografts (CDX), on the other hand, use human cancer cell lines cultured in lab conditions and implanted into immunocompromised mice. While CDX models do not fully capture human tumor complexity, their standardization and reproducibility make them valuable for fundamental research and high-throughput screening3.
Xenograft models in practice
Xenograft models are central to translational medicine attempts, as they help bridge the gap between fundamental in vitro studies and clinical trials. They provide insights into tumor biology, drug efficacy, and resistance mechanisms, supporting the development of more effective targeted therapeutic interventions such as cell therapies.
PDX models have proven useful in exploring chemosensitivity and resistance-related targets; studies have highlighted an increase in overall survival and disease-free survival in gallbladder cancer patients treated with PDX-guided chemotherapy4. Moreover, PDX models have helped researchers better understand the molecular characteristics of the cancer landscape in response to targeted therapies5,6. CDX models, on the other hand, are valuable as a primary screening tool in identifying cytotoxic drugs, which can guide further evaluation in more representative models like PDX models7.
Challenges in utilizing xenograft models
Notwithstanding the importance of xenograft models in cancer research, they come with significant challenges that can hinder their effectiveness. A key hurdle is the initial engraftment of tumor cells into mice (P0 generation). Failure at this stage means losing the sample and the opportunity to explore that specific cancer or subject model. Successful engraftment allows progression to the P1 generation to expand and stabilize the model, but failure here also results in lost potential insights8.
The disease must not only engraft but also proliferate in a manner that closely mimics the original human condition. This unpredictable factor can compromise the model’s validity. In CDX models, researchers can modify cells to express specific markers to confirm if the disease is replicating robustly and accurately, but this is not possible in PDX models.
It is common for researchers to achieve relatively low and highly variable engraftment efficiencies, limiting disease progression and increasing variability in the animals tested. For example, one study reported an overall engraftment rate of only 27.4% of 113 breast cancer patient samples9. This low efficiency often leads researchers to oversample, which is problematic. In PDX models, the available cells are frequently limited and sometimes of poor quality. While CDX models have more abundant cells, oversampling increases costs significantly due to the expensive maintenance of animal models10. The variability caused by inefficient engraftment complicates data analysis and often necessitates additional replicates, further increasing the number of animals used.
Regulatory and ethical considerations also play a critical role, particularly in regions with strict controls like the UK. Organizations such as NC3Rs advocate for reducing animal use, refining procedures to minimize suffering, and replacing animal models when possible11. In general it is best practice that researchers avoid oversampling to minimize animal usage whenever possible.
Overcoming xenograft model challenges
Achieving high efficiency in engraftment and disease progression, along with consistent disease replication across models, is crucial for reducing turnaround times, simplifying readouts, and minimizing animal use. While engraftment success hinges on a series of uncontrollable factors, such as the sample’s exposure to chemotherapy, the origin of the cells, and the tumor grade9,12,13, evidence has shown that working with highly viable cells can support engraftment, which in turn promotes more rapid disease progression14,15. By thoroughly enriching the sample for the most viable cells and removing dead cells and debris after dissociating tumor cells, toxic effects can be minimized, and engraftment efficiency can be enhanced. Not only can these improvements reduce the quantity of starting material needed per animal, but they can also lead to more effective and rapid disease progression. Ultimately, this approach maximizes the efficiency and ethical use of animals in experiments.
Enhancing xenograft efficiency with Levitation Technology
To improve xenograft model outcomes, researchers require a cell separation method that can differentiate viable cells from non-viable ones without compromising cell integrity, a challenge often presented by traditional cell separation methods like centrifugation. Levitation TechnologyTM offers a solution; it suspends cells in a paramagnetic solution within a magnetic field, effectively isolating live cells from dead cells and debris while preserving their viability. The LeviCell® system harnesses this technology to support enhanced viability and quality of cells for rodent transplantation, leading to better engraftment efficiency and disease progression. This leads to the generation of more consistent models, allowing researchers to make use of every animal they inject, improving efficiency and productivity while minimizing animal usage11.
Dr. Ernesto Diaz-Flores, Associate Professor of Oncology at the University of California San Francisco (UCSF), has successfully integrated Levitation Technology into his team’s workflow for high-risk leukemia CDX models. Previously, the research group’s workflow involved injecting one to two million cells of mixed viability into mice, achieving an 80% engraftment rate and 50% disease progression after five weeks. The LeviCell workflow reduced the number of cells needed to 100,000 at 95% viability, resulting in 100% engraftment and disease progression rates. This not only halved the time to complete engraftment from 10 weeks to five but also enhanced lab productivity and reproducibility of CDX models that accurately reflect disease heterogeneity.

To learn more about how you can improve your xenograft model generation pipelines through enhanced cell separation, get in touch with one of our experts today!
References
1. Jin J, Yoshimura K, Sewastjanow-Silva M, Song S, Ajani JA. Challenges and Prospects of Patient-Derived Xenografts for Cancer Research. Cancers. 2023;15(17):4352. doi:10.3390/cancers15174352
2. Hidalgo M, Amant F, Biankin AV, et al. Patient-Derived Xenograft Models: An Emerging Platform for Translational Cancer Research. Cancer Discov. 2014;4(9):998-1013. doi:10.1158/2159-8290.CD-14-0001
3. Souto EP, Dobrolecki LE, Villanueva H, Sikora AG, Lewis MT. In Vivo Modeling of Human Breast Cancer Using Cell Line and Patient-Derived Xenografts. J Mammary Gland Biol Neoplasia. 2022;27(2):211-230. doi:10.1007/s10911-022-09520-y
4. Zhan M, Yang R, Wang H, et al. Guided chemotherapy based on patient‐derived mini‐xenograft models improves survival of gallbladder carcinoma patients. Cancer Commun. 2018;38(1):1-9. doi:10.1186/s40880-018-0318-8
5. Russo M, Crisafulli G, Sogari A, et al. Adaptive mutability of colorectal cancers in response to targeted therapies. Science. 2019;366(6472):1473-1480. doi:10.1126/science.aav4474
6. Chen Z, Huang W, Tian T, et al. Characterization and validation of potential therapeutic targets based on the molecular signature of patient-derived xenografts in gastric cancer. J Hematol OncolJ Hematol Oncol. 2018;11(1):20. doi:10.1186/s13045-018-0563-y
7. Teicher BA. Tumor models for efficacy determination. Mol Cancer Ther. 2006;5(10):2435-2443. doi:10.1158/1535-7163.MCT-06-0391
8. Lee J, Lee G, Park HS, et al. Factors associated with engraftment success of patient-derived xenografts of breast cancer. Breast Cancer Res. 2024;26(1):49. doi:10.1186/s13058-024-01794-w
9. Yu J, Qin B, Moyer AM, et al. Establishing and characterizing patient-derived xenografts using pre-chemotherapy percutaneous biopsy and post-chemotherapy surgical samples from a prospective neoadjuvant breast cancer study. Breast Cancer Res. 2017;19(1):130. doi:10.1186/s13058-017-0920-8
10. Liu Z, Ahn MHY, Kurokawa T, et al. A fast, simple, and cost-effective method of expanding patient-derived xenograft mouse models of pancreatic ductal adenocarcinoma. J Transl Med. 2020;18(1):255. doi:10.1186/s12967-020-02414-9
11. The 3Rs | NC3Rs. Accessed May 1, 2024. https://www.nc3rs.org.uk/who-we-are/3rs
12. Byrne AT, Alférez DG, Amant F, et al. Interrogating open issues in cancer precision medicine with patient-derived xenografts. Nat Rev Cancer. 2017;17(4):254-268. doi:10.1038/nrc.2016.140
13. Jung HY, Kim TH, Lee JE, et al. PDX models of human lung squamous cell carcinoma: consideration of factors in preclinical and co-clinical applications. J Transl Med. 2020;18(1):307. doi:10.1186/s12967-020-02473-y
14. Inoue, Deem, Kopetz, Heffernan, Draetta, Carugo. Current and Future Horizons of Patient-Derived Xenograft Models in Colorectal Cancer Translational Research. Cancers. 2019;11(9):1321. doi:10.3390/cancers11091321
15. Ezquer FE, Ezquer ME, Vicencio JM, Calligaris SD. Two complementary strategies to improve cell engraftment in mesenchymal stem cell-based therapy: Increasing transplanted cell resistance and increasing tissue receptivity. Cell Adhes Migr. 2017;11(1):110-119. doi:10.1080/19336918.2016.1197480